
 Menu
Menu


Total knee replacement is one of the most familiar and well acclaimed joint replacement procedures in the field of Orthopaedics. If we talk about India, around 15 crore Indians suffer from knee related problems that drastically impact their quality of life. In fact, approximately 120,000 total knee replacement procedures are performed in India annually. A lot of patients prefer to undergo knee replacement surgery in Delhi owing to the use of highly advanced technology that helps to give unparalleled results.
The normal functioning of the knee joints is very important as our knees perform a plethora of functions that are important for maintaining a proper equilibrium in our daily life. Our knee joints move millions of times to enable us to perform various activities like walking, sitting/squatting, climbing, playing, dancing etc. without which our life would be miserable. Arthritis can drastically impact this normal functioning of the knee joints thereby giving rise to immense pain, stiffness and even deformities, which become more evident over time. All these can affect our ability to indulge in various day to day activities.
Being one of the best primary & revision knee joint replacement surgeons in Delhi, Dr Vivek Mittal has transformed the lives of numerous patients and helped them to get back on their feet without any pain or discomfort.
Knee replacement surgery is usually recommended when the knee joint is damaged beyond repair. Depending upon the extent of this damage, knee replacement procedure may vary from person to person. The various options available include:
Total Knee Replacement surgical procedure is suited best for patients whose knee joints have been completely damaged by degenerative joint issues like Osteoarthritis, Rheumatoid Arthritis, post traumatic arthritis, etc.
During the surgical procedure, the affected joint is supplanted (replaced) by a prosthetic joint that is created specially to fit in. The artificial joint is properly cemented into the place to negate any risks of dislocation or loosening. Over 95% of the patients with severe knee pain and stiffness have shown considerable improvement after the surgery and most are able to walk 24 hours after surgery, thoughwith the help of walking aid initially.
Total knee replacement gives you freedom of movement by relieving symptoms like pain and stiffness, correcting the deformity by the use of prosthetics and deterring the need of using a wheelchair or walker. The surgery helps the patients to return close to their normal lifestyle and continue their day to day activities which had to be, otherwise, frequently put on hold due to extreme joint pain.
Total Knee Replacement not only enhances the quality of your life but also gives you the freedom of movement by allowing you to return to your routine activities, attend social functions, enjoy holidays, etc.
Total knee replacement gives you “freedom from pain & movement for life” by providing relieffrom excruciating pain, stiffness, swelling, instability anddeformity. It also gives you freedom from walking aids such as wheelchair or walker. Knee replacement surgeryenhances the quality of life by helping you regain your life and activities which were put on hold due to debilitating knee arthritis.


Knee Osteotomy is a good alternative to total knee replacement surgery in a young or middle-aged patient suffering with unicompartmental arthritis of the knee joint.
A normal joint has a good cartilage and thick meniscus and it allows body weight to pass equally through both the condyles of the knee joint. However, as the arthritis progresses, the cartilage on one side of the knee joint wears faster than the other side, causing the deformity of the leg. If the inside or the medial side of the joint is worn then a varus deformity (bow-legged) will develop. On the contrary a valgus deformity results (knock-knees) when the outside, or lateral side, of the joint is worn. Deformity redirects the burden of our body weight only through the damaged condyle of knee while the healthier part of the knee is spared. Over a period of time this vicious cycle leads to the progression of the arthritis.
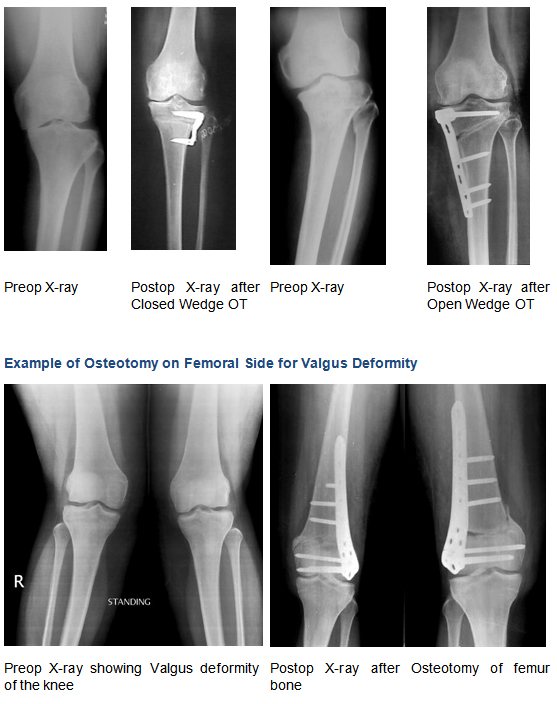
Osteotomy means surgically breaking the bone under control condition. It can be done on femur bone for knock-knee deformity or on tibia bone for bowleg deformity. An osteotomy realigns the bone into a better position, it shift the weight-bearing forces to the healthier condyle of the knee joint, thereby “unloading the worn side’ of the joint.
Osteotomy of tibia bone is done for varus deformity of knee, while femur osteotomy is done for valgus deformity. Either osteotomy can be done by close wedge method or open wedge method.
For the operation to be effective the arthritis needs to be confined to one area of the knee only, and the rest of the joint must be healthy. The ideal patient for a knee osteotomy is a young, active person, who has arthritis limited to one side of the knee joint causing significant pain, disability and deformity.
The other criterion is the ability of patient to cooperate with non-weight bearing ambulation and rehabilitation for 8-10 weeks.
However, before suggesting an osteotomy, one must try physiotherapy, anti-inflammatory medication and, if necessary, keyhole surgery to control symptoms.
Patient must understand when bone is cut, it needs time to heal, and therefore, rehabilitation from this surgery is lengthy and may be difficult if you are not prepared for it. The total healing time is 8 – 12 weeks, and can take longer. Most patients need physical therapy to regain their knee motion.
The osteotomy can improve the symptoms of knee arthritis but cannot cure the disease, hence will fail with time, and total knee replacement eventually will be required.
Sometimes overcorrection or under correction of deformity is possible. Other potential complications include problems with healing of the osteotomy (a nonunion), continued pain from arthritis, blood clots, and infection.
When done in the right patients, knee osteotomy is usually successful at decreasing pain caused by arthritis. Osteotomy can delay conversion to knee replacement from few years to over a decade.
“Because of this, knee osteotomy is generally reserved for young, active patients, who want to delay the time until knee replacement”
Unfortunately, performing this surgery in the wrong patient can have poor outcomes. Even though many people want to avoid knee replacement surgery, the knee osteotomy is not right for everyone.
Patients generally should not consider this surgery if they have:
As the osteotomy is fixed with a plate, plaster cast is not necessary; rather a removable knee brace is sufficient for 2 – 3 weeks. Most patients are ready to go home after 3 – 4 days. You will need a walker to ambulate toe touch non-weight bearing for 6 – 8 weeks. Knee bending will be allowed and when you are comfortable. Progressing weight bearing is allowed thereafter depending on your x-ray.
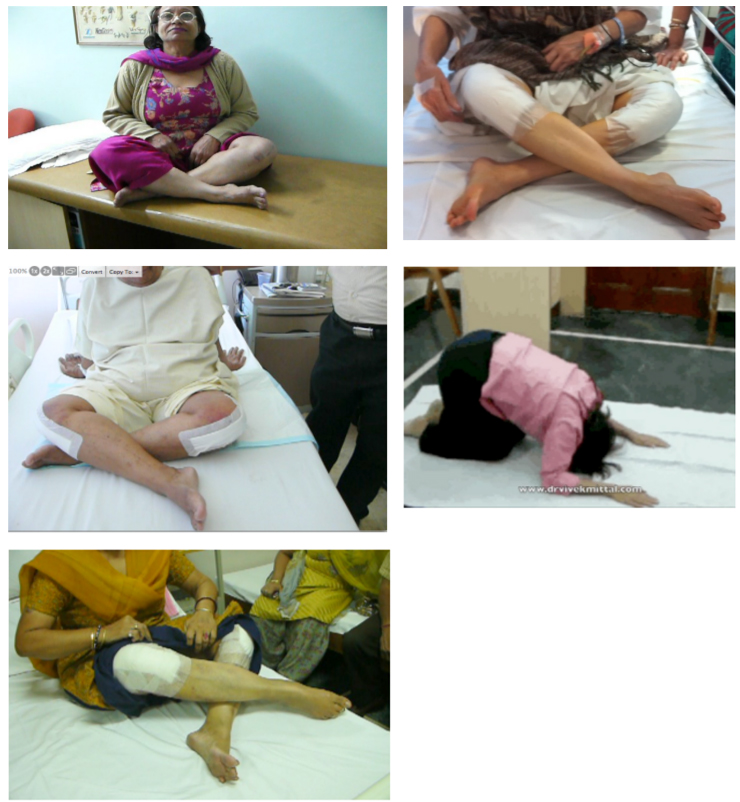
The advantage of osteotomy over knee replacement in the younger patient is that once it has healed, it allows you to lead a busy, vigorous life and even returning to sports. In our social circumstances, sitting cross leg and squatting on the floor is allowed, but only after osteotomy has healed.

Total knee replacement is a highly successful operation. It corrects the deformity, allows painless mobility, gives you independence and improves quality of life. Conventional Total Knee Implants, however, allows knee flexion up-to 120 degrees to 125 degrees
Many daily activities require the ability to bend the knee beyond 125 degrees. Climbing stairs,for example, requires a range of motion from 75–140 degrees while sitting in a chair and standing up again requires a 90–130 degrees range of motion. Other activities, like gardening, playing golf or kneeling for prayer involve motions that require up to 130–150 degrees of flexion to perform. Many societies or culture demand certain activities requiring high flexion. Certain favorite activities of yours may also require higher flexion as well like gardening etc.
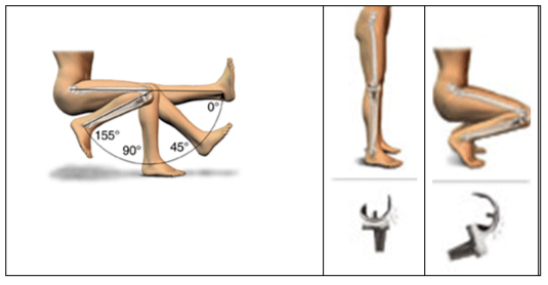
So far sitting cross-legged on the floor was not advisable after conventional Total Knee Replacement. The various High Flexion Implants are specifically designed to safely accommodate deep flexion upto 150 – 155 degrees. Therefore, it is now possible to sit cross-leg or squat after High Flexion Total Knee Surgery. However, it is important to realize that the ability to sit cross-leg and squat does not only depend on the implant or the surgeon, but to an extent on patients as well, whether they had similar ability before surgery. Patients with pre-operative good range of motions and muscle strength after appropriate physiotherapy can post operatively resume an active life style including deep flexion for religious, cultural, recreational activities.
Most important factor for choosing High Flexion Total Knee Replacement is pre-operative good range of motions including capability of high flexion before the surgery. Other factors include early and intensive physiotherapy after surgery necessary to regain deep flexion, besides weight and activity level of the patient. The principles of high flexion knee replacement are quite similar to conventional knee replacement. You should discuss with your Orthopedic surgeon whether the High Flexion Fixed Knee Replacement is the appropriate option for you.

As with any major surgery, there are potential risks involved after Total Knee Replacement surgery. Even though the incidence of complications after Total Knee Replacement are small, yet their significance is high for both Patient as well as surgeon, considering the complexity of the procedure. The decision to proceed with any surgery is made because the advantages of surgery outweigh the potential disadvantages. It is important that you are informed of these risks before the surgery takes place.
Complications can be medical (general) or local complications specific to the Knee.
Medical complications include those of the anesthesia as well as your other illness related, almost any medical condition can occur so this list is not complete. Few of them include:
Infection
Infection can occur after any operation. Being a foreign body artificial joints are always at more risk of infections especially with any dental work or other surgical procedures where germs (Bacteria) can get into the blood stream and find their way to your implant. Although infection rates after joint replacement surgery are very low (approximately 1%), yet, even this percentage is very significant.
Lot of precautions is taken before & during surgery to prevent this complications, which includes preoperative part preparation, blood test & urine test, Antibiotics, Sterile operation rooms with laminar airflow etc. Patients with Diabetes, Rheumatoid arthritis, Psoriasis, Renal & Hepatic Compromised patients, HIV patients, h/o past infection like TB, Chronic urinary tract infection, etc. are at a higher risk for developing postoperative infections.
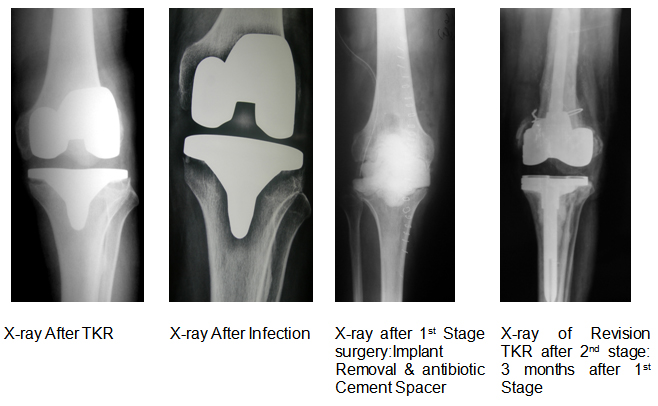
Early infections and low virulence infections can be treated with antibiotics, but may require further surgery like surgical debridement (joint cleaning), if they do not respond to antibiotics alone. If infection persist or gets aggravated in spite of adequate antibiotics / joint cleaning then your artificial joint may need to be removed and replaced by cement antibiotic spacer to eradicate infection.
If you have any unexplained pain, swelling, or redness in the operated knee joint, you should consult your surgeon as soon as possible.
Blood Clots (Deep Venous Thrombosis)
Blood clots in the veins of the legs are one of the most common complications of total knee replacement surgery. They can form in the calf veins and can travel to the lung (Pulmonary embolism). Pulmonary embolism is serious and even life threatening complication. It is treated with medicines to dissolve it. Adequate precautions are taken before & after surgery to prevent them from occurring; like LMWH (medicines), Aspirin, Calf pumps, early exercises, Stockinet’s etc. Blood clots can occur despite all these precautions and are usually not dangerous if appropriately treated. If you get calf pain or shortness of breath at any stage, you should notify your surgeon immediately.
Stiffness in the Knee
Ideally, your knee should bend as much as before surgery but on occasion, may not bend even, as much as, was present before surgery. For unexplained reasons, some patients form excessive scar tissue in the knee after surgery, resulting in diminished bending of the knee (a condition called arthrofibrosis). It is impossible to predict ahead of time which patients might develop arthrofibrosis. In these patients manipulation of the knee is required to break down the excessive scar tissue, this means going to the operating room where the knee is bent for you while under anesthesia. Arthroscopic surgery to clean up the excessive scar within the knee joint may be required, rarely if nothing helps.
Ligament Injuries
There are a number of ligaments surrounding the knee. These ligaments can be torn during surgery or break or stretch out any time afterwards. Ligament injury to inside of the knee (medial collateral ligament) can be of serious consequence requiring reoperation.
Patellar Complications
Occasionally the kneecap does not track properly on the femoral component causing it to “jump” as the knee bends. The chance of this occurring is very less with the current generation of total knee implants. The plastic part on the patella can wear through. These problems sometimes need reoperation for correction.
Damage to Nerves and Blood Vessels
Rarely these can be injured at the time of surgery and are debilitating. Nerves and blood vessels run very close to the knee joint. Nerve damage can (rarely) occur with knee replacement. The most common nerve damaged is the nerve to the muscles that bring the foot up toward the face (the peroneal nerve). The odds of this occurring are very low. If it does occur, the affected nerve usually recovers after 6 to 12 months. Quite commonly the skin around the knee feels “numb” because of small skin nerves that get cut at surgery. Sensation usually returns to normal within a few months. Arterial injury is an uncommon but serious complication. The major arteries of the leg lie just behind the knee joint. Once injured, blood vessels are explored and repaired by a vascular surgeon. If not, you could even lose your leg. The chance of this occurring is extremely small.
Fractures or Breaks in the Bone
Incidence of such fractures is low. Fractures or breaks can occur during surgery in severely osteoporotic bones. Sometimes patient also develop stress fracture around knee without any fall especially those with severe deformity and who delays surgery for long. These fractures can be managed successfully during the surgery with special implants. Sometimes fractures are noticed only on post operative x-rays, and they are managed by modifying postoperative rehabilitation protocol or rarely may requires resurgery.
Fracture around the implant (peri-prosthetic fractures) can happen many weeks or months after the surgery. These peri-prosthetic fractures usually require surgery.
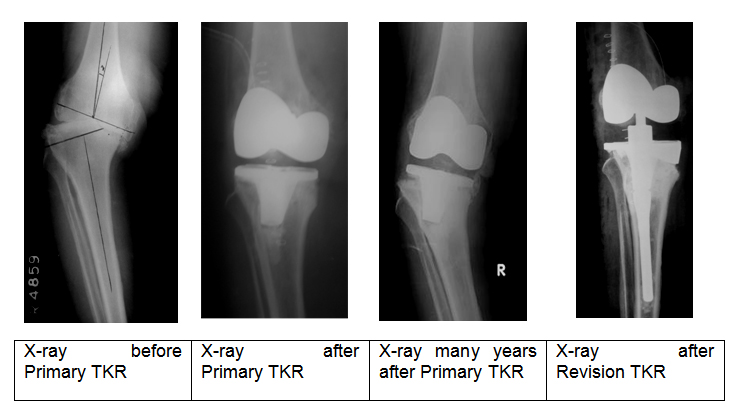
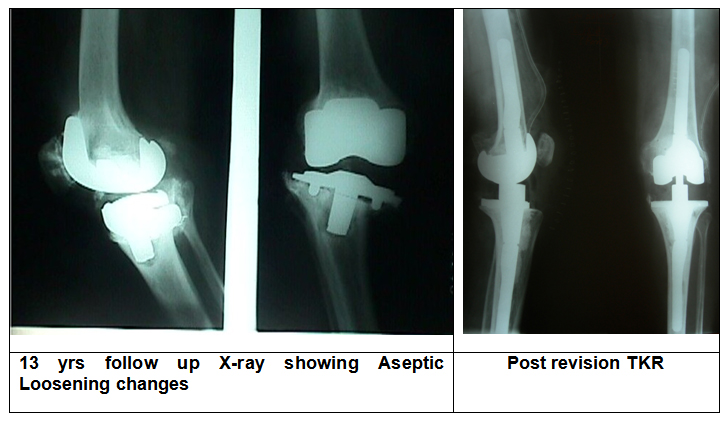
Aseptic Loosening
It is the most important long-term problem & the reason for revision of total knee replacement surgery. Loosening of the prosthesis from the bone is the most important long-term problem. Current generations of implant have good survivorship. Good surgery, choice of correct implant with proven design and good survivorship, maintaining good quality of bone & muscle, maintaining weight and avoiding high impact activities are some of the factors which delay this complication. As implants gets loose & bone quality & quantity becomes poor, Revision Total knee Replacement surgery is the ultimate solution.
Cosmetic Appearance
The knee may look different than it was because it is put into the correct alignment to allow proper function.
Leg length Inequality
This is most likely to happen when a patient with significant deformity of both knees chooses to undergo one knee operation at a time. This happens due to the fact that a corrected knee is straighter and hence longer.
Dislocation
An uncommon complication where the ends of the knee joint lose contact with each other or the plastic insert may come out of tibial base plate. This requires reduction under anesthesia, however surgery is needed for reduction of dislocation of plastic, and sometimes for dislocation of knee.
Allergy to the Metal Parts of Implant
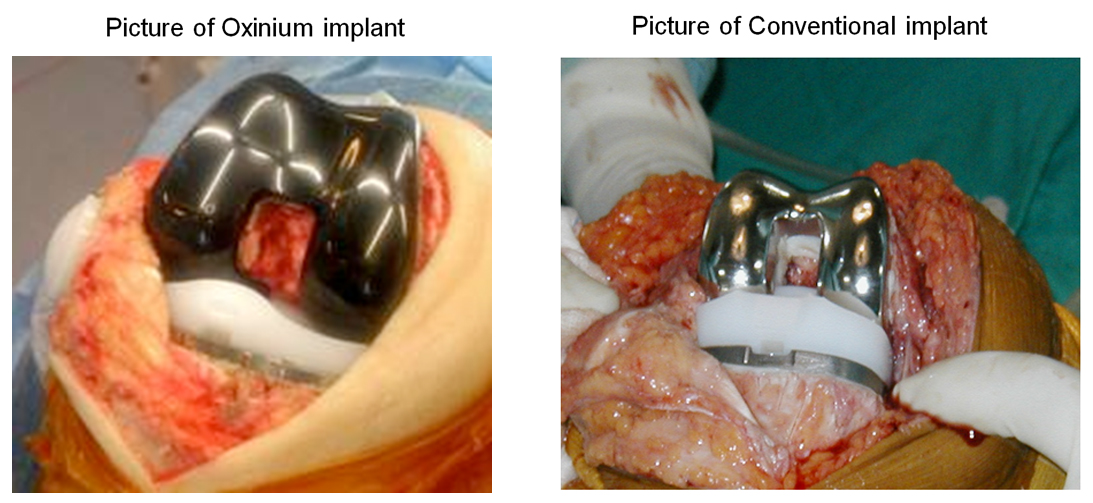
Allergy to the metal parts of the implant has occasionally been reported. People who know they have metal allergies should mention to their surgeon before surgery. Metal allergies are rare and also the tests are not completely reliable. Oxinium Total Knee implant is completely inert and can be successfully implanted in these patients.
Summary
I understand surgery is not a pleasant prospect for anyone, but for some people who are crippled with arthritis, it could mean the difference between leading a near normal life and putting up with a debilitating condition.
Surgery is only offered once non-operative treatment has failed. It is an important decision to make and ultimately it is an informed decision between you, your surgeon, and your family. Surgery offers correction of knee deformity, relief in pain, and restoration of movements to bring independence in all the activities important for daily living. With recent advances in medicines and anesthesia this is done with the least amount of possible risk.
Although most people are extremely happy with their total knee implant, complications can occur and you must be aware of these prior to making a decision. You should discuss all of your concerns thoroughly with your Orthopedic Surgeon prior to surgery so that you can be sure that this is the procedure for you.

What is a partial knee replacement?
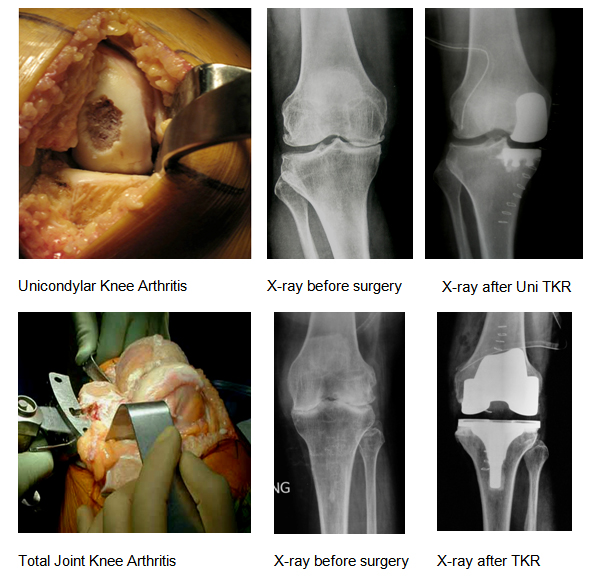
Most people are aware of total knee replacement surgery. However, many of these patients have arthritis limited to one part of the joint. To make you understand better, assume knee joint is a three-compartment structure: an inside compartment, an outside compartment, and a front compartment. The inside and outside compartments are between thigh and leg bones while front compartment is for thigh bone and kneecap articulation.
To start with, many middle-aged men and women develop osteoarthritis of only the inner half or medial compartment of the knee joint (also called medial compartment osteoarthritis) which proceeds to affect the outer half or lateral compartment and knee cap compartment later.
In Unicondylar knee replacement, only that part of the knee, which is unhealthy and arthritic, is replaced, rather than the entire surface of the knee joint. The normal surfaces are left alone.
The Unicondylar knee arthroplasty provides lasting pain relief to those younger patients who have debilitating knee pain as a result of unicompartmental osteoarthritis, but are too young for a total knee replacement.
What can patients expect after this procedure (advantages of Unicondylar knee arthroplasty)?
For patients suffering from single compartment arthritis, Unicondylar knee replacement offers many benefits over a total knee arthroplasty.
Unicondylar knee replacement patients not only have less pain but also have speedy recovery (less time in the hospital) after surgery and achieve greater range of motion (sitting cross legged and squatting) sooner than patients treated with total knee arthroplasty. The need for blood transfusion is rare.
Unicondylar knee replacement can be done through a mini incision thereby further improving the outcome.
Last but not the least even if Unicondylar knee replacement fails or implant is worn out early, a total knee replacement surgery can be done without difficulty.

Are there any disadvantages of Unicondylar knee arthroplasty?
The major disadvantage of Unicondylar knee replacement is the inferior long-term survivorship in comparison to total knee replacement. At times the results are not as good as total knee replacement.
Diagnosis
There is no blood test to diagnose Osteoarthritis of knee joints, however, blood tests are done to rule out infection, rheumatoid arthritis or other inflammatory arthritis.
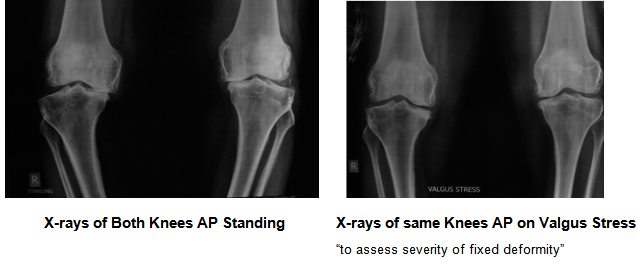
The diagnosis of osteoarthritis is made on history, physical examination & X-rays of both the knee joints AP (Standing), Lateral and Stress views (to see if deformity is correctible).
Am I a candidate for Unicondylar Knee Replacement?
Careful patient selection is critical for unicompartmental knee arthroplasty. This is a good procedure for either younger patients (around 50 yrs) or elderly patients (70 – 80 yrs) having predominantly single compartment degenerative / osteoarthritis and preferably having weight less than 100 kg. No significant degenerative changes in the other compartments should be present, and both cruciate ligaments should be intact.
Other criteria’s includes passively correctable malalignment of the limb to neutral and not beyond. Thus you should preferably have varus deformity less than 15° or a valgus deformity less than 20°, or flexion deformity less than 15°. Your knee should have good range of motion before operation.
Who is not a good candidate for Unicondylar Knee Replacement?
Unicondylar knee replacement should not be considered if you have one of the following:
How do I prepare for my surgery?
Preparation for surgery is in part patients (i.e. yours) and in part your surgeons’ job. First you have to prepare your self for the surgery mentally, and understand its outcome, its pros and cons. Your commitment as a patient is very important for the successful outcome of surgery.
Surgeons’ evaluation starts by ensuring that your knee is the cause of your disability and is damaged severely enough to warrant surgery. At times, affliction from spine or hip joint can simulate knee pain and partial knee replacement will fail to relieve your pain in these situations.
In history, your pain is assessed, any prior knee injuries or problems like infection or inflammatory arthritis are looked into, your activities of daily living are noted, and the need of pain-killers or any drug allergies are recorded. We will also be discussing your other medical history with you to assess the risk during surgery.
A physical examination will identify your knee’s range of movement, deformity, and alignment. A standing X-ray of both knees from front (AP) and supine X-ray of both knees from side (Lat) will help evaluate the extent of damage and deformity in your knee. Stress X-rays are also taken to assess the extent of fixed deformity in your knees.
You may be subjected to blood tests, an MRI (magnetic resonance imaging scan), or a bone density scan if required.
We recommend surgery when non-surgical treatments like lifestyle changes, medication, injections and physical therapy have been exhausted. Surgery can provide you adequate relief of pain and good functional recovery to return to the best possible quality of life.
What is the Surgical Procedure?
Surgery is performed under sterile conditions in the operating room mostly under spinal or combined spinal and epidural anesthesia. It takes 30 – 45 minutes to prepare the knee. Surgery is performed under a tourniquet and surgical time per knee is usually 35 – 45 minutes.
The leg prepared with a sterilizing solution and draped under aseptic precautions. An incision is made to expose the knee joint. The bone ends of the femur and tibia are prepared using a saw. Trial components are inserted to assess fitting of the components, alignment of the leg, stability and range of movements of the knee joint.
The Final components (Femoral & Tibial) are then put into place with cement and then knee is closed over drains and finally dressed and bandaged.

What is a revision knee replacement?
Revision knee replacement surgery is a procedure in which a previously implanted prosthesis is revised or replaced with a new total knee implant. An original total knee implant has four components; femoral, tibial, plastic insert and patellar component.
A revision total knee replacement can be a revision of all the components or revision of one component, for example only change of polyethylene (plastic) liner.
Revision total knee replacement surgery is a demanding surgery, but the results are good in the vast majority of patients, though not as good as primary total knee replacement surgery.
When is it needed?
Total knee replacement surgery is a highly successful surgery with a good long-term result of 95% at 15 yrs. It provides dramatic relief in pain, correction of deformity, improvement of functions and independence in the life of patients suffering with advance arthritis of the knee. Not only this surgery is being done in ever increasing numbers, but also it is now offered to younger and active individuals who subject there replaced knee joints to high demands, affecting its longevity and leading to failure.
A loose knee implant tends to be painful and unstable, therefore patients who wear out their prosthesis will require a revision knee replacement surgery. Approximately 5% to 10% of knees undergoing TKA will require revision within 10 to 15 years.
Knee replacements can wear out for a variety of reasons. Polyethylene wear has emerged as an important cause of TKA failure (aseptic loosening and Osteolysis (development of loose bone cavities around hip implant without loosening of implant)). The most common indications for revision TKA are infection, mechanical loosening, and instability. Dislocations, Periprosthetic Fractures (breaking of the bone around the prosthesis),
A case of polyethylene wear leading to loosening
All revision total knee replacement other than for infection is done in single stage. In the case of infection, the primary implant may need to be removed to treat the infection, an antibiotic spacer need to be inserted along with few weeks of antibiotics, and once infection is controlled then revision knee replacement is performed.
How do I know when I need revision surgery?
If your pain is increasing, if you are feeling instability or having difficulty in walking or you have to use a support for walking, if you are noticing loss of mobility in the knee joint, or there is continuous discharge from the operative scar not responding to any treatment, then its time for you to consult your doctor for the possibility of revision knee replacement
Sometimes may have few or no symptoms, but your x-rays show a big osteolysis next to the implant, which may be indicative of a need for revision surgery. Some other times you are very symptomatic, and x-rays also show gross malalignment or loosening of components or change in the position of components or you has sustained with periprosthetic fracture.
The decision and extent of revision knee replacement depends on severity of discomfort, x-rays, blood investigations like CRP or ESR and patients overall clinical condition. At times patient is required to undergo special investigations like Tc99 Bone scan / I111 bone scan or MRI to confirm the diagnosis. It is essential to remove a loose or damaged prosthesis before irreversible harm is done to the joint and surrounding bone.
Underlining the complex nature of surgery, the right time for revision knee surgery can be decided by you together with your Orthopedic surgeon in consultation with Physician and Anesthetist.
If you a revision knee surgery, you must discuss your options with your Orthopedic surgeon.
How revision total knee replacement can help me?
The revision total knee replacement surgery is a successful and durable operation, but not as much as primary total knee replacement surgery. You can expect significant improvement in your symptoms after revision knee surgery, which includes:
How different is revision knee surgery different than primary total knee replacement?
The principles of revision TKA are similar to those of primary surgery. However, revision knee surgery is more challenging and complicated than primary knee replacement. Poor quality of the patients bone often makes it difficult to achieve stable fixation of revision knee implants. Furthermore, removing the previous knee implants not only necessitates more extensive surgery, but also adds to loss of bone to the already limited patient bone stock.
Also not only do the patients tend to be older, but also the surgery time is longer and the blood loss is greater during or after surgery adding to the difficulty of revision surgery. Together, these problems make revision knee replacement much more complex surgery.
Revision knee surgery on an infected knee requires two or more separate operations. In the first operation, the old knee prosthesis is taken out and a block of cement mixed with high dose of antibiotics (antibiotic spacer block) is inserted in the joint for 6 – 12 weeks. This block acts as a spacer and also releases high concentration of antibiotics in the knee joint locally. The patient is also given intravenous antibiotics for 6 weeks, and constantly evaluated with repeated TLC, DLC, CRP and ESR. After the infection has cleared, the knee is reopened and the new revision prosthesis is implanted.
A case example of Management of infected TKR
During the revision surgery one may need special implant like constraint knees or rotating hinge with wedges, blocks, cone sleeves, extension rods, etc. Though these implants are expensive and have some limitations, but indispensable (in certain situation) to achieve good stability of revision implant.
What should I expect during my hospital stay?
Before Surgery: Most of the patients are admitted two days before surgery and undergo a through medical checkup which includes evaluation by the treating surgeon, anesthetist, intensivist, and physiotherapist besides investigations like Chest X-rays, ECG, blood (including CRP, ESR, TLC & DLC) and urine test. X-ray images of knees from different angles are taken to plan your surgery. You may require whole body bone scan or MRI of the knee. At least 2 – 3 units of blood may be necessary. Careful control of blood sugar is done before surgery.
Knees are scrubbed with soap and water, painted with betadine solution, and then covered with a sterile drape in your room a night before your operation.
Surgery: Preferable choice of anesthesia is Spinal anesthesia (it anesthetize both legs only) with sedation. The duration of surgery ranges from 2 to 3 hrs. You will be kept in a recovery room for one day for the monitoring of vital parameters. Knee bending is started on an exercise machine after 2-3 days of operation.
After Surgery: On the 3rd day your drainage tubes will be removed while on 4th day your dressing will be changed. In most cases a knee immobilizer will be worn. Knee bending on the CPM machine is started 2-3 days after surgery; bedside sitting is started on the 4th day while walking with support and toilet training are started from 5th day onwards.
Most patients can ambulate comfortably with the support of a stick or walker, bend knee up to 800 to 900, start going to toilet and are also able to climb a flight of stairs. Most patients are comfortably discharged on 8th to 10th day.
What happens after I go home?
Aftercare following knee revision surgery is essentially the same as for knee replacement, consisting of a combination of physical therapy, rehabilitation exercises, pain medication when necessary, and a period of home health care or assistance.
You will be requiring antibiotics for a longer time as compare to primary total knee replacement surgery especially if you are a diabetic, rheumatoid arthritis patient or infection was the cause of revision knee surgery.
The recovery time after revision knee replacement surgery depends on the cause of revision and may vary from 4 to 8 weeks.
What are the risk following Revision Total Knee Replacement?
The complications following revision knee surgery are similar to those for knee replacement and include:

S Box High Flex Knee Replacement
High Flexion Total Knee Replacement is a good option for people having good pre-operative range of movements. Many patients with severe deformity are still able to sit cross-legged before surgery. Conventional Total knee replacement is a highly successful operation but usually allows knee flexion up to 1200 to 1250.
Many daily activities require knee movements beyond 1250. They include sitting or kneeling for prayers, climbing stairs, sitting cross-legged, etc. Many societies or culture demand certain activities requiring high flexion.
High Flexion Implant is specifically designed to safely accommodate deep flexion up to 1500 – 1550. Therefore, it is now possible to sit cross-leg or squat after High Flexion Total Knee Surgery.
However, it is important to realize that the ability to sit cross-leg and squat does not only depends on implant alone but choosing the right patients as well. Patients with pre-operative good range of motions and muscle strength after appropriate physiotherapy can post operatively resume an active life style involving deep flexion movements for religious, cultural and recreational activities.
S Box JOURNEY TKR
The JOURNEY Bi-Cruciate Stabilized knee system is designed to offers better function of stability, strength, and movement and feels like a normal knee, because unlike conventional knee systems, this implant design replicates the functions of both the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL).
The JOURNEY Bi-Cruciate Stabilized Knee System addresses many of the problems associated with conventional TKA systems. The JOURNEY Bi-Cruciate Stabilized Knee System is well suited for high demand, or active patients, and offers patients good movement and function to the patients.
The JOURNEY Bi-Cruciate Stabilized System is also available in OXINIUM material, although, it adds to the cost, but on the other hand it provides superior benefit of less wear.
S Box OXINIUM TKR
Over the years, after proven success of Total Knee Replacement, more younger and active patients are opting for this surgery. This not only necessitates improvement in the longevity of the implant but also enhancement in their performance.
Oxidized Zirconium (Oxinium) has been introduced as a revolutionary new material for articulating surface in total joint replacement. Oxinium knee has shown great reduction in the wear of plastic insert (by up to 85% in lab settings). Oxinium has superior biocompatibility as compared to cobalt-chromium implant, and Oxinium implants are safe in patients suffering with metal sensitivity, as they do not contain significant levels of Nickel.
S Box Revision Knee Replacement
Like revision total hip replacement surgery is a demanding surgery, and the challenges are same and includes poor quality of bone, more extensive surgery, more blood loss, requirement of special implants and sometime surgery in stages. However, the results are good in the vast majority of patients, though not as good as primary total knee replacement surgery.
Replaced Knee can wear out for a variety of reasons. Polyethylene wear (aseptic loosening) is the leading cause of long term TKA failure. Other common indications for revision TKA are infection, mechanical loosening, and instability. Dislocations (if repeated), Periprosthetic Fractures (breaking of the bone around the prosthesis) can also require revision knee surgery.
It can be a revision of all the components or revision of one component, for example only change of polyethylene (plastic) liner. Also sometime treatment other than direct revision knee replacement may be necessary. For example, in the case of infection, the knee implant may need to be removed to treat the infection, an antibiotic spacer need to be inserted along with few weeks of antibiotics, and once infection is controlled then revision hip replacement is performed. Similarly for fracture around the prosthesis, fixation of fracture by plate may suffice.
S Box Uni Knee
Knee joint is a three-compartment structure, two between thigh and leg bone and one between thigh and knee-cap bone.
In Unicondylar knee replacement, only that part of the knee joint (between thigh and leg bone), which is unhealthy and arthritic, is replaced, rather than the entire surface of the knee joint. The healthy part of the joint is left alone.
The Unicondylar knee arthroplasty provides good pain relief to those younger patients who have debilitating knee pain as a result of unicompartmental osteoarthritis, but are too young for a total knee replacement.

Over the years Total Joint Replacement is being performed in younger and more active patients. This necessitates improvement in the longevity of the implant and enhancement in their performance.
Most current femoral components in total knee replacements are made of metal (cobalt–chromium) with plastic (polyethylene) as an articulating surface. Excellent results are currently being achieved with this material, more so in elderly population. Over a prolonged period, these implants can roughen up in the body. When the femoral component then rubs over the plastic (polyethylene) insert (abrasive motion), the plastic surface starts to wear out or break up due to generation of plastic debris. The rougher the femoral surface, the worse the amount of wear. The plastic wear particles or ‘debris’ produced by this motion can cause Aseptic Loosening, the most important cause of failure of total knee replacement. Aseptic Loosening happens not only due to the thinning of the plastic insert itself but also due to the body’s reaction to the microscopic plastic debris particles which can cause loosening and thinning of bone at the implant interface.
What is Oxinium and what are the key advantages of Oxinium?
In recent years, oxidized zirconium (OxZr) has been introduced as a revolutionary new material for articulating surface in total joint replacement. Oxinium is produced as a result of oxidation of zirconium metal thereby changing its surface property from metal to ceramic, which is harder and smoother than cobalt-chromium and has reduced wear by up to 85% in lab settings. Oxinium also has improved frictional characteristics, and excellent biocompatibility as compared to cobalt-chromium implant.
Unlike conventional cobalt-chromium implant, Oxinium implants are safe in patients suffering with metal sensitivity, as they do not contain significant levels of Nickel.
If you feel that we can be of any assistance please take a moment to fill out the enquiry form below and one of our staff members will answer your question as soon as possible.
Follow us on social media and keep up to date with all the latest news from the Dr vivek mittal clinic.
