What is a partial knee replacement?
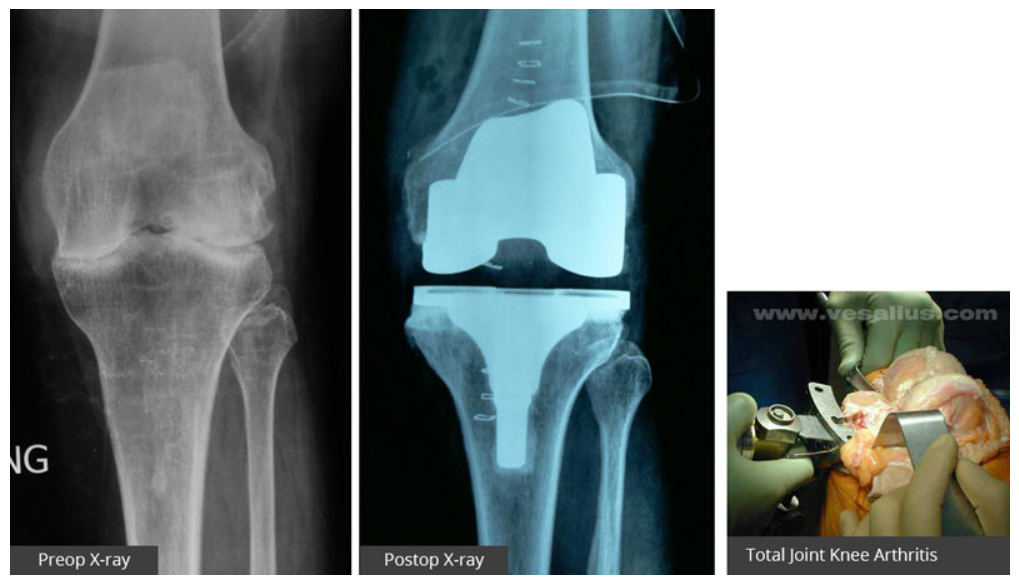
Most people are aware of total knee replacement surgery. However, many of these patients have arthritis limited to one part of the joint. To make you understand better, assume knee joint is a three-compartment structure: an inside compartment, an outside compartment, and a front compartment. The inside and outside compartments are between thigh and leg bones while front compartment is for thigh bone and kneecap articulation.
To start with, many middle-aged men and women develop osteoarthritis of only the inner half or medial compartment of the knee joint (also called medial compartment osteoarthritis) which proceeds to affect the outer half or lateral compartment and knee cap compartment later.
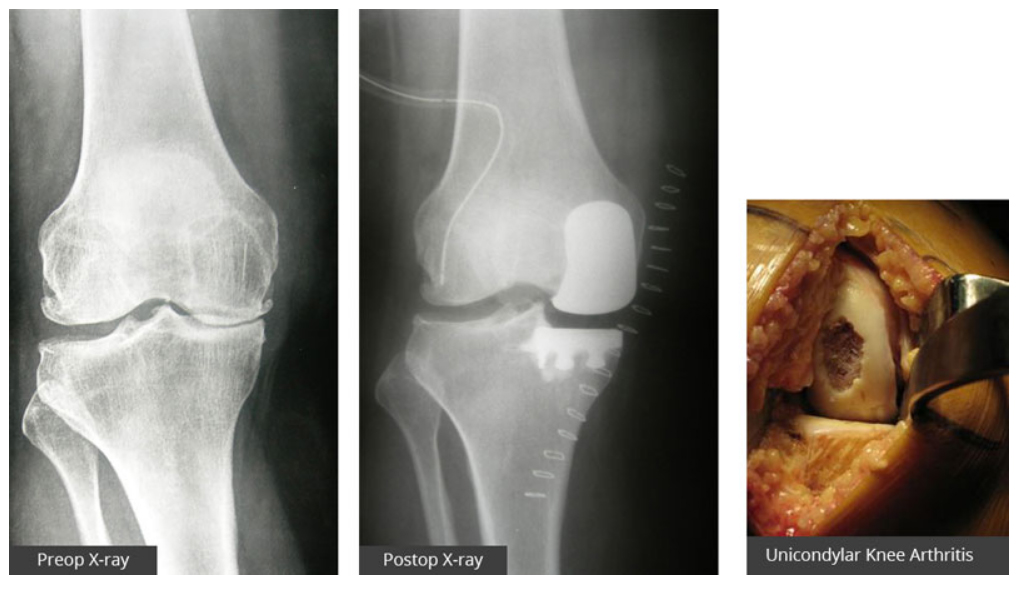
In Unicondylar knee replacement, only that part of the knee, which is unhealthy and arthritic, is replaced, rather than the entire surface of the knee joint. The normal surfaces are left alone.
Dr Mittal Total Knee Replacement
The Unicondylar knee arthroplasty provides lasting pain relief to those younger patients who have debilitating knee pain as a result of unicompartmental osteoarthritis, but are too young for a total knee replacement.

What can patients expect after this procedure (advantages of Unicondylar knee arthroplasty)?
For patients suffering from single compartment arthritis, Unicondylar knee replacement offers many benefits over a total knee arthroplasty.
Unicondylar knee replacement patients not only have less pain but also have speedy recovery (less time in the hospital) after surgery and achieve greater range of motion (sitting cross legged and squatting) sooner than patients treated with total knee arthroplasty. The need for blood transfusion is rare.
Unicondylar knee replacement can be done through a mini incision thereby further improving the outcome.
Last but not the least even if Unicondylar knee replacement fails or implant is worn out early, a total knee replacement surgery can be done without difficulty.
Are there any disadvantages of Unicondylar knee arthroplasty?
The major disadvantage of Unicondylar knee replacement is the inferior long-term survivorship in comparison to total knee replacement. At times the results are not as good as total knee replacement.
Diagnosis
There is no blood test to diagnose Osteoarthritis of knee joints, however, blood tests are done to rule out infection, rheumatoid arthritis or other inflammatory arthritis.
There is no blood test to diagnose Osteoarthritis of knee joints, however, blood tests are done to rule out infection, rheumatoid arthritis or other inflammatory arthritis.
Am I a candidate for Unicondylar Knee Replacement?
Careful patient selection is critical for unicompartmental knee arthroplasty. This is a good procedure for either younger patients (around 50 yrs) or elderly patients (70 – 80 yrs) having predominantly single compartment degenerative / osteoarthritis and preferably having weight less than 100 kg. No significant degenerative changes in the other compartments should be present, and both cruciate ligaments should be intact.
Other criteria's includes passively correctable malalignment of the limb to neutral and not beyond. Thus you should preferably have varus deformity less than 15° or a valgus deformity less than 20°, or flexion deformity less than 15°. Your knee should have good range of motion before operation.

Who is not a good candidate for Unicondylar Knee Replacement?
Unicondylar knee replacement should not be considered if you have one of the following:
- Infection
- Inflammatory Arthritis / Rheumatoid Arthritis
- Stiff knee (restricted range of motion)
- Incompetent Cruciate Ligament
- Involvement of all the three compartments
- Morbidly Obese patient
How do I prepare for my surgery?
Preparation for surgery is in part patients (i.e. yours) and in part your surgeons' job. First you have to prepare your self for the surgery mentally, and understand its outcome, its pros and cons. Your commitment as a patient is very important for the successful outcome of surgery.
Surgeons' evaluation starts by ensuring that your knee is the cause of your disability and is damaged severely enough to warrant surgery. At times, affliction from spine or hip joint can simulate knee pain and partial knee replacement will fail to relieve your pain in these situations.
In history, your pain is assessed, any prior knee injuries or problems like infection or inflammatory arthritis are looked into, your activities of daily living are noted, and the need of pain-killers or any drug allergies are recorded. We will also be discussing your other medical history with you to assess the risk during surgery.
A physical examination will identify your knee's range of movement, deformity, and alignment. A standing X-ray of both knees from front (AP) and supine X-ray of both knees from side (Lat) will help evaluate the extent of damage and deformity in your knee. Stress X-rays are also taken to assess the extent of fixed deformity in your knees.
You may be subjected to blood tests, an MRI (magnetic resonance imaging scan), or a bone density scan if required.
We recommend surgery when non-surgical treatments like lifestyle changes, medication, injections and physical therapy have been exhausted. Surgery can provide you adequate relief of pain and good functional recovery to return to the best possible quality of life.
What is the Surgical Procedure?
Surgery is performed under sterile conditions in the operating room mostly under spinal or combined spinal and epidural anesthesia. It takes 30 – 45 minutes to prepare the knee. Surgery is performed under a tourniquet and surgical time per knee is usually 35 – 45 minutes.
The leg prepared with a sterilizing solution and draped under aseptic precautions. An incision is made to expose the knee joint. The bone ends of the femur and tibia are prepared using a saw. Trial components are inserted to assess fitting of the components, alignment of the leg, stability and range of movements of the knee joint.
The Final components (Femoral & Tibial) are then put into place with cement and then knee is closed over drains and finally dressed and bandaged.

 Menu
Menu
